By Erika Koutroumpa,
Oral health is defined as the health of the mouth including the head, face and oral cavity. The mouth is one of the most useful tools that a human can possess since it is used in major functions – breathing, eating and communicating with others. Having a healthy mouth ensures its proper function for many years to come and is essential to maintaining a good quality of life. Yet, in most countries, this part of healthcare is neglected and often there is limited access to it. World Oral Health Day is an initiative led by the World Dental Federation (FDI), beginning in 2007. Its aim is simple: to raise awareness about the importance of oral healthcare at an international level.
Looking at the statistical records of the past few years, it becomes evident why such an initiative would take place. According to WHO, oral–related illnesses affect more people worldwide than mental disorders, cardiovascular disease, diabetes, chronic respiratory disease and cancers combined and as seen in the organization’s Global Oral Health Status Report (2022), oral diseases affect close to 3.5 billion people worldwide. Based on the Global Health Index, untreated tooth decay in adult teeth is the most common health condition with approximately 2 billion people being afflicted. Tooth decay is the destruction of the organ’s hard tissues due to the accumulation of bacterial biofilm on its surface, in severe cases leading to loss of function and even inflammation and tooth loss. Gum (periodontal) disease is mainly the result of infections and inflammation of the gums and bones that surround and support the teeth, and it is among humanity’s most common diseases, affecting up to 50% of the global population. Furthermore, the estimated global prevalence of edentulism (complete tooth loss) is almost 7% in people aged 20 years old and older, while it is most common in the age group of 60 years and older (23%). Lastly, oral cancer is ranked as the 13th most common worldwide, accounting for 3,777.713 new cases and 177,757 deaths in 2020 alone.

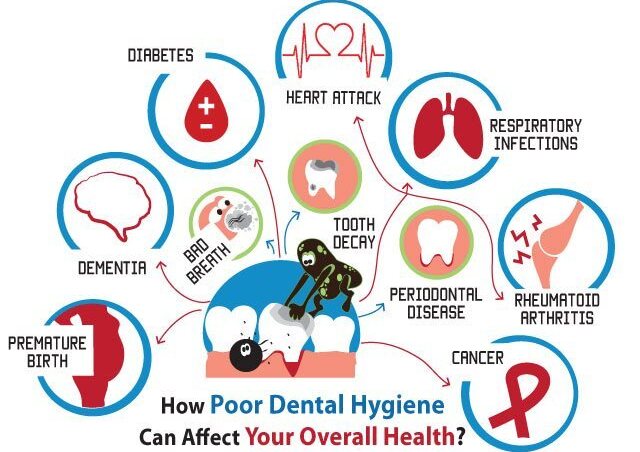
Poor oral health has a significant impact on a person’s quality of life. Its implications affect essential human functions, such as the ability to eat and speak, may cause disturbances in sleep and lack of focus on everyday activities, hence impacting academic and work performance, but also create poor self–esteem and exclusion from social circles. Not only that but oral diseases have been interlinked with systemic ailments. Specifically, periodontal disease has been associated with diabetes, metabolic syndrome, obesity, eating disorders, liver disease, cardiovascular disease, Alzheimer’s disease, rheumatoid arthritis, adverse pregnancy outcomes and cancer. As a result, it is of pivotal importance to keep such issues under control.
“Oral health has long been neglected in global health, but many oral diseases can be prevented and treated with the cost–effective measures outlined in this report,” said WHO Director–General, Dr. Tedros Adhanom Ghebreyesus. “WHO is committed to providing guidance and support to countries so that all people, wherever they live and whatever their income, have the knowledge and tools needed to look after their teeth and mouths, and to access services for prevention and care when they need them”. But this is easier said than done since oral healthcare is characterized by great inequalities. Most countries in the world do not include dental healthcare in their healthcare coverage and all the treatments are undertaken by private dentists, resulting in high out–of–pocket expenditures, the results of which can be catastrophic. Hence, a huge burden of oral diseases and conditions affects the most vulnerable and disadvantaged populations.
According to the Global Burden and Inequality of Dental Caries, from 1990 to 2019 globally, 64.6 million and 62.9 million prevalent cases of caries in permanent and deciduous teeth were due to inequalities due to socioeconomic factors 2019. People on low incomes, people living with disabilities, older people living alone or in care homes, those living in remote and rural communities and people from minority groups carry a higher burden of oral diseases. Only a small percentage of the global population is covered by essential oral health services, and those with the greatest need often have the least access to services. This pattern of inequalities is similar to other non–communicable diseases such as cancers, cardiovascular diseases, diabetes and mental disorders. Risk factors common to noncommunicable diseases such as high sugar intake, all forms of tobacco use and harmful use of alcohol all contribute to the global oral health crisis.
Most oral health diseases are multifactorial – multiple different parameters can lead to their manifestation. However, most of them can be altered, so the risk of illness can be significantly reduced. Public health initiatives usually target these influences, which can also influence the progression of other systemic diseases — the common risk factors. This includes the cessation of smoking and drinking, promoting a balanced diet low in free sugars, community water fluoridation and encouraging the use of protective equipment when doing sports or traveling via bicycles or motorcycles. Developing more effective oral health interventions and policies, although highly possible, is inhibited by poor information and surveillance systems and low priority for public oral health research. Community water fluoridation is one of the most important public health policy measures against oral diseases, as it can substantially reduce the risk of dental caries. However, it still remains inaccessible in many parts of the world with a limited number of countries have implemented it.
The WHO argues that oral health care should be part of universal health coverage, “either free of charge or at a price that people can afford,” adding that too many people do not have access to needed dental care. A resolution on oral health was passed in 2021 at the 74th World Health Assembly. As an ambitious next step, in 2022 the Geneva–based NGO adopted the global strategy on oral health, aiming to include Universal Health Coverage for oral health in the goals for 2030. “Placing people at the heart of oral health services is critical if we are to achieve the vision of universal health coverage for all individuals and communities by 2030” , said Dr. Bente Mikkelsen, WHO Director for Noncommunicable Diseases. But there is still a lot that remains to be done,and great efforts should be expected in order to turn this dire state around.
To conclude, taking care of one’s oral health is important not just for aesthetics – a nice smile can go a long way when it comes to proper systemic health and a good quality of life. The lower the socioeconomic level of a person, the poorer their oral health, meaning that community–wide efforts are key elements to improving the current state of oral health globally. After the initiation of WHO’s efforts towards integrating dental care into universal health coverage, great change in the sector is expected. But until the goals fully materialize, civilians should take matters of their oral care into their own hands, the easiest way being twice–daily tooth brushing with fluoride–containing toothpaste (1,000 to 1,500 ppm) and by visiting their dental healthcare provider at least every once a year for a checkup.
References
- Oral health-key facts. who.int. Available here
- “Global Burden and Inequality of Dental Caries, 1990 to 2019”, P.Y.F. Wen, M.X. Chen, H.M. Wong, Journal of Dental Research, Volume 101, Issue 4
- World Health Organization cites ‘alarming’ dental statistics. washingtonpost.com. Available here
- Key facts about oral health. fdiworlddental.org. Available here
- Kapila Y. L. (2021). Oral health’s inextricable connection to systemic health: Special populations bring to bear multimodal relationships and factors connecting periodontal disease to systemic diseases and conditions. Periodontology 2000, 87(1), 11–16